41y old man with altered sensoriuM
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen :
A 41yr old man who is a farmer came with complaints of pain abdomen and vomitings since one day
Patient was apparently alright 2 days back later he had pain abdomen following an acute binge of alcohol(750ml of local liquor) in epigastric region, colicky type,non progressive, non radiating,Which got relieved on taking food
He had vomitings-2 episodes, non bilious,non projectile,contents being food particles
No H/o fever, loose stools, melena, abdominal distension, constipation, burning micturition, head trauma
PAST HISTORY:laprotomy done 10 yrs back for peptic ulcer perforation
Not a k/c/o HTN, DM, CAD, epilepsy,CKD
HABITS: He was on mixed diet, normal appetite, bowel n bladder regular
Chronic alocholic since 10-12 yrs-initially 350ml per day later 750ml local liquor every day
Toddy intake 1-2 bottles if liquor not available
Chronic smoker since 10 yrs Beedis—1pack/day
Cravings for alochol and tobacco chewing present
GENERAL EXAMINATION:
Pt is conscious, irritable and confused(GCS-13/15) moderately built and nourished
No Pallor,icterus, cyanosis, clubbing, lymphedenopathy, pedal edema
VITALS: febrile-100 degree celsius
BP: 160/100mm hg
Pulse:80bpm
RR-28cpm
PER ABDOMEN- shape of abdomen-scaphoid
CVS-s1 s2 heard, no murmurs
RS- BAE clear, no added sounds
CNS- pt is agitated and confused and was restrained
Not co operative so could not perform cns examination and MMSE
TREATMENT:
1 NBM till further orders
2 IV fluids
3 INJ PANTOP 40mg OD
4 INJ TRAMADOL 1 amp in 100ml NS BD
5 INJ THIAMINE 1 amp in 100ml NS TID
6 INJ LOREZEPAM 4mg slow IV /6th hrly
7 INJ HALOPERIDOL 5mg im/sos
8 GRBS 6th hrly
9 BP/temp/PR 4th hrly
10 I/O charting
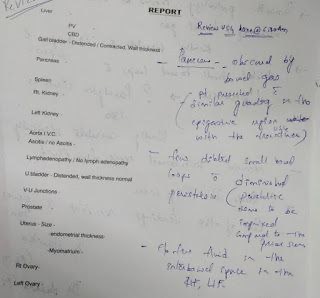
PROVISIONAL DIAGNOSIS:?ACUTE PANCREATITIS
? ALCOHOL WITHDRAWAL SYNDROME
? DELIRIUM TREMENS
?WERNICKE’S ENCEPHALOPATHY
umbilicus - inverted , soft, tenderness +, no guarding , no rigidity,no organomegaly, bowel sounds hear




Comments
Post a Comment