Medicine Blog
I am an intern in medicine department and one of the important terms of getting the internship completion is to complete my log book with my daily log of what I learn during the course of my duties.
CASE:
A 65 year old man presented to the ER with a chief complaint of weakness in both his lower limbs since 15 days.
Detailed History
The youngest of 2 and timid and shy as a boy, he quit school at an early age in 7th standard and pursued farming and other hard labor, following his father's footsteps. His early work involved shepherding, breaking stones and lifting heavy weights. He was renowned for his prowess in his locality. Married at the age of 20, he has 3 children with two daughters and a son (attendant). A few years after his marriage, into his early 30s, the patient first reported exertional, pounding palpitations associated with a heaviness in his chest. He remembers that this subsided when he took rest for a while. At this point he did not have any dyspnea, cough, chest pain, syncope or pedal edema. His palpitations were initially occasional, about once in 2 to 3 months and started gradully progressing when he felt them as frequently as once a week, 5 years after initial onset. He precisely remembers that at this point, he felt breathless for the first time, which was unusual for his hard day's labor. The patient reports that this breathlessness progressed over several years, into his early 50s, when he felt dyspneic even on walking for short distances. Dismayed that he may have lost his once famous prowess, the patient had to quit work. Due to his decreased work capacity and consequently reduced financial returns, he shared a terse relationship with his wife which made him frequently visit his elder sister for emotional comfort and shelter. He was still able to get some menial jobs and fend for himself and his children. However, 5 years ago at age 60, the patient's son reported that his father suddenly woke up from sleep one day, gasping for breath with profuse sweating. He said that he had to stand for a while and walk around for the breathlessness to relieve. The patient reported that this only ever happened twice in his life. He denied a history of orthopnea or pedal edema at any point. He did not have a history of syncope, hemoptysis, fever or migratory joint pains at any point. He also denied chest pain. No history of hoarseness of voice either.
With these symptoms badly limiting his functional status, the patient's consumption of alcohol increased significantly, which was previously occasional (about once a month, where he used to drink himself to a blackout) to a state where he drank almost daily, 90ml of cheap whiskey.
He says that poor nutrition, with hard labor and increased alcohol intake gradually caused him pains with troubling pain in his knees and low back. On one unfortunate day when was indulging himself to a black out, he tripped and fell and injured his right hip region. This was 5 years ago and since then the patient had been taking a painkiller (possibly NSAID) almost everyday, either orally or injectables for 5 years now.
His life was more or less along the same lines when 15 days ago, he complained to his son that he had difficulty in getting up from bed and from a sitting position. Squatting became very difficult. He also reported severe aching pain in his lower limbs, more on the left side than right. He did not report of any contractures or muscle atrophic changes. No history of cramps or exercise induced pains. His fatigue worsened over these past 15 days. Over the course of these 15 days, the weakness progressed to a level where he was absolutely unable to get up from bed 4 days ago. He was also unable to lift his hands above his head without difficulty. He also couldn't support himself without hands on the bed when sitting. He however did not complain of any difficulty in mixing food or buttoning his shirts. The patient did not report any tingling or other paraesthesias anywhere or any numbness. He said that he felt the surface on which he was walking. He also had no history of his footwear slipping or a high stepping stride. Overall he says that both pain and weakness are more in his left LL than right LL. Although he did not report it, his son told us that he was unable to comb his hair without difficulty.
At this point after listening to his history our differential was
? Myopathy
Physical examination findings to follow:
Patient was concious coherent and cooperative,thin built and moderately nourished.
No pallor,icterus, cyanosis, clubbing and pedal edema
Afebrile
PR:76bpm,high volume pulse
BP:130/70 mm Hg
Systemic examination:
CVS:S1 S2 heard
Duroziez sign positive
Pulsus bisferiens positive
RS:BAE present
NVBS heard
ABDOMEN:
Soft non tender
No organomegaly
Bowel sounds present
On CNS examination:
-Higher motor functions are intact
-Tone :Normal in both upper limbs and reduced in both lower limbs
-Power in upper limbs are 4+ and lower limbs rt:3/5 lt:0/5
-Reflexes:
Biceps,
triceps,
supinator,
knee are in present
Ankle is absent
Plantars:Extensors
-Beevor's sign:positive
-Sensory examination:Fine and crude touch,pain and temperature are preserved;
Vibration and proprioception are lost in lower limb and intact in upper limb.
-Cranial Nerve examination is normal
-Tenderness is present in dorsal and lumbar region
Since the patient had even lose of prioprioception and vibration with extensor plantar response Myeloneuropathy was our provisional diagnosis
Investigation
(1) ECG:The ECG is regular with a heart rate of 69 bpm
(2) Xray chest:Chest xray shows no significant findings
(3)Hemogram:
Hb - 8.8g/dl
TLC - 6300 c/cumm
Platelets - 2.32 L/cumm
(4)CUE:
Alb +
Sug -
Pus Cells 5-6/hpf
epi cells 4-5/hpf
(5)RFT
UREA:49 mg/dl
CREATININE:1.0mg/dl
URIC ACID :4.4mg/dl
CALCIUM:9.7mg/dl
PHOSPHOROUS :3.7mg/dl
SODIUM:141mEq/L
POTASSIUM: 3.7mEq/L
CHLORIDE:101mEq/L
(6)LIVER FUNCTION TEST (LFT)
Total Bilirubin-1.05 mg/dl
Direct Bilirubin-0.37 mg/dl
SGOT(AST)-19 IU/L
SGPT(ALT) -10 IU/L
ALKALINE PHOSPHATE-356IU/L
TOTAL PROTEINS-6gm/dl
ALBUMIN-3.7gm/dl
AG RATIO-1.71
(7)2D ECHO:
EF IS 55 %
Dilated IVC OF 1.9CM,
Dilated RA
RSVP-38MMHG
Mild TR with mild PAH, Trivial AR
Good LV systolic function,
No RWMA Diastolic Dysfunction
(8)Serum CK 36 IU/L
(9)RPR was done to rule out the possibility of Tabes Paresis
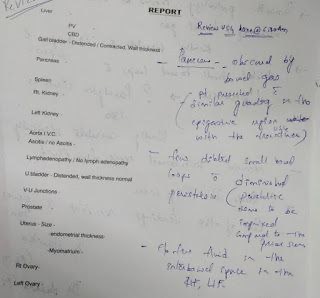
(10)Ultra Sound
Since he has urinary symptoms and has grade 2 prostatomegaly we took a urology consultation and got a dre done
Dre revealed a flat and non nodular prostate.
Diagnosis:
Myeloneurpathy secondary to spinal cord compression which is ? vertebral Metastatic lesions at D8,D10 And L2
Treatment Given
1.INJ THIAMINE 1 AMPULE IN 100ML NS/IV/BD
2.INJ OPTINEURON 1 AMPULE IN 100ML NS/IV OD 3.TAB CIPROFLOXACIN 500 MG PO/BD. 3 DAYS
4.SYRUP LACTULOSE 20 ML PO/BD
PSA to be done to rule out prostatic malignancy.





Very well put and presented. Looking forward to more posts.
ReplyDeleteThankyou Mam..!!
Delete