Medicine
Hi this is intern posted in General Medicine department and one of the important terms of getting the internship completion is to complete my log book with my daily log of what I learn during the course of my duties.
Here is a case i have seen:
CASE HISTORY
28 year old man, civil engineer from Coimbatore, first child born out of a non consanguinous marriage to a Civil engineer and housewife. He was born and brought up in Coimbatore. He has 2 younger sisters, the elder one is in her btech final year and the younger one is in her btech first year. He finished his engineering 5 years back after which he started working in Chennai. He was completely asymptomatic 1 year back, when he felt very tired one evening after his daily 8am to 5pm routine, he got better after resting for 2 days after which he resumed his daily activities. He moved to Nalgonda and started working at Pamalagula. 20 days back he says he had chicken biryani at a Dhaba 1 week after which he started having non projectile, non bilious, non blood tinged vomitings containing food content, he had an episode of vomiting each time he consumed food or even water. He avoided consuming food to avoid these episodes of vomitings. He visited a local RMP practitioner first after 3 days of onset, he was prescribed a tablet for 2 days after which he vomitings subsided on the 4th day. He again started having vomitings from the 5th day after which he went back to the same practitioner who gave him a tablet which relieved his vomitings for the day. The next morning on day 6, he continued having around 8-9 episodes of vomitings after which he went to Laxmi hospital in Nalgonda where he was put on IV fluids.
He felt better for a day but he started observing high coloured urine and he felt dyspneic even on walking for few steps.
His attendant says that the patient has lost weight over the past one month.
Other than that the patient gives no history of body pains, joint pains, easy fatiguability, cola colored urine, dark coloured stools
No complains of fever, pain abdomen, night sweats
No complains of drug intake such as NSAIDs, antibiotics, anti malarials
No family history of similar episodes
No history of blood transfusions
PERSONAL HISTORY:
Diet : mixed
Sleep: adequate
Bowel and bladder : regular
GENERAL EXAMINATION:
Patient is Conscious coherent and cooperative
,moderately built and moderately nourished.
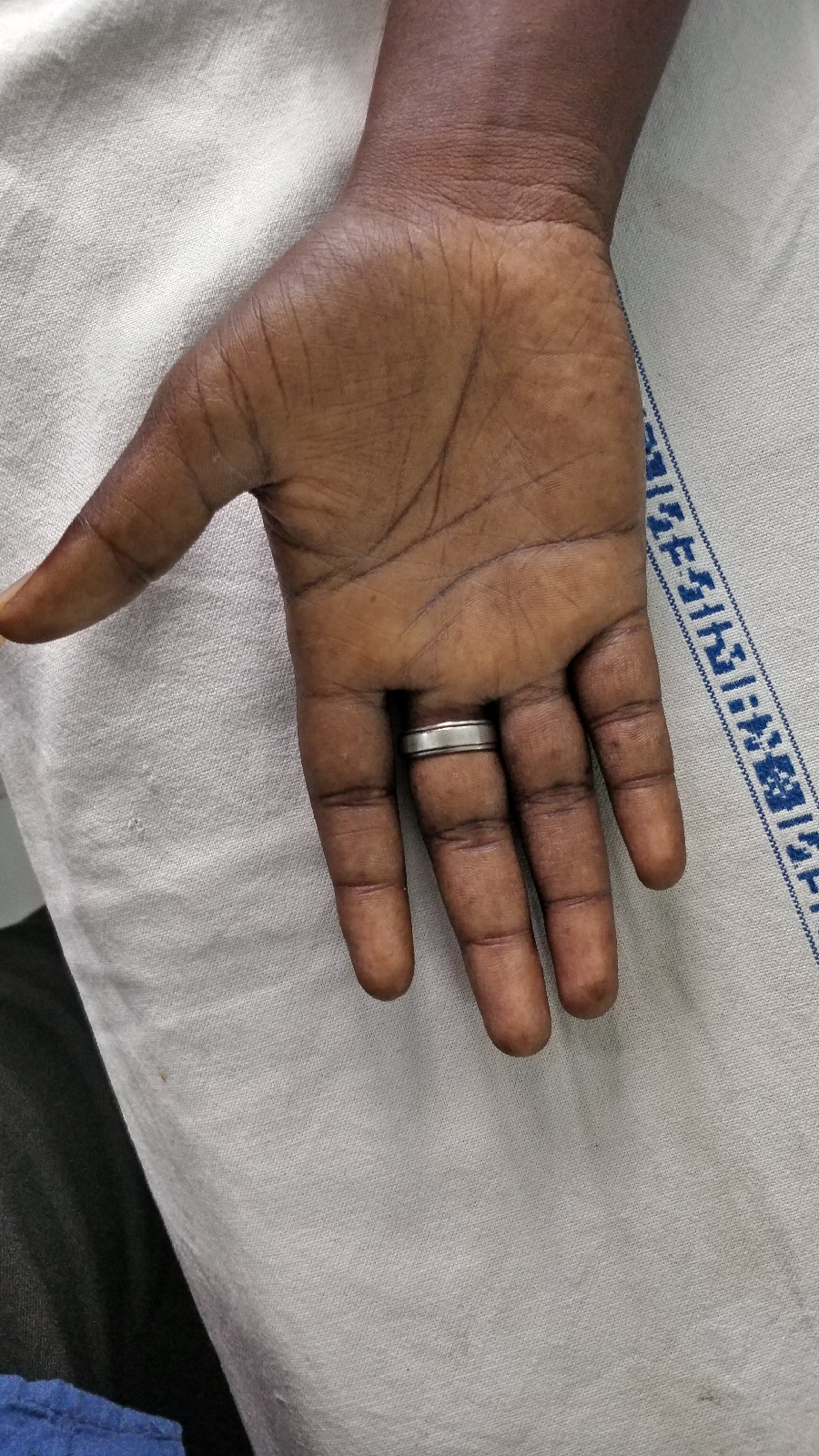
Pallor +
No cyanosis,clubbing,
lymphademopathy,edema
PR- 88bpm
RR- 18cpm
BP - 120/60
Temp - 98.4
Saturation -98%
P/A -
Soft
Non tender
Bowel sounds +
Cvs - apex beat half inch from MCL
S1, S2 +
Lungs - clear
P/A of non-tender
CN-NAD
CHEST X-RAY
ECG
HEMOGRAM
Hb: 5.0
TLC 4200
Neutro- 52
Lympho-46
PCV-14.1
MCV- 96.9
MCH- 34.3
MCHC- 35.4
RBC- 1.45
Plt- 1.3 lakh
RETICULOCYTE COUNT-2.6
CORRECTED RETIC COUNT-0.9
PERIPHERAL SMEAR-
Normocytic normochromic with mild hypochromesia few microcytes with anisopoikilocytosis tear drop cells ovalocytes.
The peripheral smear shows no schistocytes, spherocytes, bite cells
LDH=5142 IU/L
RFT
Urea- 45
Creat- 0.7
UA- 6.1
Ca++: 10
Phosphorus-5.0
Na+ 137
K+ 4.8
Cl- 94
LFT:
TB- 2.94
Direct bilirubin- 1.04
AST 124
ALT 30
ALP 85
TP 6.1
ALBUMIN 4.5
A/G 2.96
ABG
Ph-7.42
Pco2-35.6
Po2-87.6
Hco3-23.1
Tco2-51.2
st.Hco3-23.8
o2sat-96.4
o2 count-6.6
Anti Hcv-Non reactive
HbsAg- Negative
HIV 1/2-Non-reactive
Serum Lipase-41
Serum amylase-35
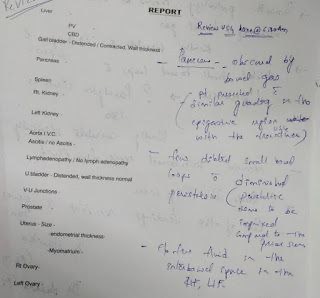
USG- no sonological abnormalities detected
Sample sent for Coombs test and Osmatic fragility test
reports awaited.
Diagnosis-
1.?Haemolytic anemia.
2.? Nutritional anemia secondary to vit b12 or iron deficiency.
2.Acute Gastritis.
Treatment
1. IVF-NS DNS @100ml/hr
2. INJ.PANTOP 40mg/IV/OD
3. INJ.ZOFER 4mg /iv/tid
4. Inj.Optineuron 1amp in 100ml NS/IV/OD
5. Vitals monitoring.
Hemolytic anemia could be inherited or acquired.
It can be extracorpuscular or due to intracorpuscular defects.
Inherited intracorpuscular defects could be due to hemoglobinopathies, enzymopathies, membrane defects where as extracorpuscular factors could be familial HUS
Acquired intracorpuscular defected could lead to PNH and extracorpuscular factors are mechanical destruction, toxic agents, drugs, infections





Hi Rakesh,
ReplyDeleteGood blog.
There are a few discrepancies in the history where you say that the patient has not been able to consume anything because it is leading to vomiting and yet in his personal history, you say his appetite is intact. So does that mean an intact appetite with inability to consume or a complete loss of appetite.
The attendant says that the patient appeared to lose weight and yet down below you mentioned that there was no complaint of weight loss.
Also the PR on manual count was 88 and the ECG is showing a HR of 100. It is significant and needs to be clarified.
What would your pivot point be in this case ? The Anemia or the subacute vomiting ?
It's also extremely unusual for a patient with 10 episodes of vomiting per day to not have any signs of dehydration, electrolyte abnormalities or AKI. The history needs to be taken again I guess.
DeleteOsmotic fragility test ? For Hereditary Spherocytosis? What is the pretest probability of it being positive ? No splenomegaly either.
Delete